 When people think mental illness, they think Depression, Anxiety, Bipolar, schizophrenia and many more. But people forget that Postnatal Depression (PND) is a mental illness. From speaking to friends who have experienced Postnatal Depression they have been blamed for the illness or have been ignored by family members. Postnatal Depression is not a normal part of child birth. To me this is infuriating, especially as I have seen people go through this. One mother told me that there doctor refused to refer her to local Community Mental Health Team (CMHT) as ‘Postnatal Depression is hormonal and can be treated with medication’. This really doesn’t help with the feeling of they are the one at fault.
When people think mental illness, they think Depression, Anxiety, Bipolar, schizophrenia and many more. But people forget that Postnatal Depression (PND) is a mental illness. From speaking to friends who have experienced Postnatal Depression they have been blamed for the illness or have been ignored by family members. Postnatal Depression is not a normal part of child birth. To me this is infuriating, especially as I have seen people go through this. One mother told me that there doctor refused to refer her to local Community Mental Health Team (CMHT) as ‘Postnatal Depression is hormonal and can be treated with medication’. This really doesn’t help with the feeling of they are the one at fault.
The Facts[i]
In the UK
- Approximately 33% of mothers who experienced depression symptoms during pregnancy went on to have PND.
- Approximately 25% of mothers still suffered from PND up to a year after their child were born.
- Approximately 58% of new mothers with PND did not seek medical help. This was often due to them not understanding the condition or fearing the consequences of reporting the problem.
- 33% of new mothers with more than one child reported suffering from PND; of this group, 54% sought professional treatment
- 26% of first-time mothers reported suffering from PND; of this group, 42% sought professional treatment
These facts are shocking and sad. It shows clearly that people need educating about Postnatal depression. Especially, because of the emotional damage and the bond between mother and child, and for the rest of the family unit.
So what is Postnatal Depression.
Being a mother can bring stress, worry and anxiety. Approximately 80% of new mothers go through a period of depression[ii] which is brief and manageable, called ‘baby blues’, or deeper and long term, called ‘Postnatal Depression . ‘baby blues’ disappear within a week or so, whereas Postnatal Depression symptoms are longer lasting and can sometimes interfere with day-to-day life. Symptoms can include feeling an inability to connect with or look at the new baby, and feeling too anxious to interact with friends and family[iii].
The charity 4Children says that it considers new mothers to have Postnatal Depression if they experience three or more of the following symptoms. Experiencing five or six is considered Severe Postnatal Depression[iv]:
- Low mood/miserable most of the time
- Constantly exhausted
- Feeling unable to cope
- Feeling guilty about not being able to cope or not loving the baby enough
- Overwhelming anxiety about the baby
- Tearful for no reason
- Difficulty in sleeping
- No appetite or the urge to eat
- Difficulties in bonding with the baby
- Difficulties in their relationship with their partner
- Low energy levels
- Low sex drive
- Withdrawal from family or friends
The most serious form of Postnatal Depression is Puerperal Psychosis (otherwise known as Postpartum Psychosis). It is an extremely severe but rare form of Postnatal Depression, affecting around two in 1,000 women. It tends to present itself within a few days after childbirth, manifests in erratic and delusional behaviour by the new mum and requires urgent hospital treatment. The symptoms of Puerperal Psychosis include: confusion and disorientation, hallucinations, delusions, paranoia and lack of insight and awareness[v].
Why don’t people seek treatment?
It is important for society and health professionals to be aware of the symptoms of Postnatal Depression and its most severe form Puerperal Psychosis. We also need to realise why people don’t seek help so we can treat suffers better and encourage them to seek treatment where they are treated with dignity and respect. Importantly, reassure the mother that it is not their fault, that it is an illness.
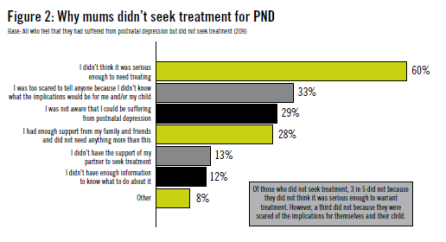 Shockingly 60% percent of those with Postnatal Depression didn’t think it was serious enough to seek treatment. Sadly 33% were too scared to tell anyone because they didn’t know what the implications would be for them and/or their child. 29% didn’t know that they were suffering from postnatal depression.[vi]
Shockingly 60% percent of those with Postnatal Depression didn’t think it was serious enough to seek treatment. Sadly 33% were too scared to tell anyone because they didn’t know what the implications would be for them and/or their child. 29% didn’t know that they were suffering from postnatal depression.[vi]
Theses statistics speak for themselves. I think it is sad that mothers are fearful of what would happen to them and their children. And that those didn’t think it was serious enough or didn’t even realise they were suffering from postnatal depression. It clearly shows that that more needs to be done to raise awareness of Postnatal Depression and reduce the stigma associated with the illness. It doesn’t help that the Media only reports cases where a mother, child or even both, have been put in sever dander or have sadly lost there lives. It is important to remember that those with mental health problems are more a danger to themselves. it is rare that children lose there lives, and if it does happen it is because of sever neglect from the services that are trained to intervene and protect lives.
It is encouraging that 28% said that they had enough support from family and friends, that they felt this was enough for them to overcome Postnatal Depression[vii].
But so much more needs to be done to prevent Postnatal Depression, and to support those with postnatal depression.
Living with Postnatal depression
A young mother, Grace, shares her experience of Postnatal Depression.
‘I can’t really put it into words what it’s like to have Postnatal Depression, because as some mental health issues you don’t always know that you have it. I was in a long term relationship (we both worked full time jobs) and even my partner didn’t see how much I was struggling inside. My behaviour changed, I wasn’t taking care of my little boy like I should have as a young mum. It was almost like I put a barrier up, blocking all feeling and ultimately feeling numb, not just towards my son to everyone and everything and as much as I tried to ‘pull myself together’, however it’s not as easy as that.’
‘Having a traumatic birth have to say I think this had a main contributor in my illness. Because of my illness, I couldn’t look after my son and I couldn’t even look after myself.
My relationship broke down I moved back to my parents and my partner had my son full time. I also lost my full time job as a waitress because I couldn’t cope with the simplest of thing without bursting into tears and panic attacks constantly.’
‘I coped by getting drunk and consequently got me into all sort of trouble. When I eventually went to my GP he diagnosed me with postnatal depression. I was put on some anti depressants, and sent on my way. I felt rejected by my GP. However, I didn’t take them because i was told by people about their affects on my health and addictions to anti depressants. So I did not take them and continued to get worse.’
Sadly for grace it got to the point where she could barely function, and returned to her GP.
‘It got to the point where I would only leave my bed for a drink or to use the bathroom. I there was little else I could do. Even washing was too much for me. I eventually returned to my GP and was immediately referred to counselling. I also had my medication changed a few times. Eventually my Mum, not knowing what to do phoned the Doctors who advised me to go voluntary into a mental health unit, or be sectioned, as I was a risk to myself.’
However, grace found that being in a mental health unit helped her on her way to recovery.
 ‘In the unit, I was given more help and talking therapy. I also to some lovely people some of whom is still keep in touch with. I was discharged after three weeks. When I left the unit, I walked out the door happier and heather with the right medication it also changed my whole perception of mental illness! It really was an eye opener.’
‘In the unit, I was given more help and talking therapy. I also to some lovely people some of whom is still keep in touch with. I was discharged after three weeks. When I left the unit, I walked out the door happier and heather with the right medication it also changed my whole perception of mental illness! It really was an eye opener.’
‘Life now has changed forever, I feel guilty every day for what I put my family, friends and most of all, my son, and the stress I put them through. All I can do from here if hope people forgive and forget and enjoy my wonderful life.’
For those reading this if you take something from this story, it would be to reach out for help. Grace would like to you to see how quickly things can escalate, and urges people suffering to help.
‘Mental health has massively increased People need to know mental health illnesses because one day it could save someone and get them to a ‘safe’ place. I think all I have been through there was a purpose for it. It was unnecessary for my life to crumble but I honestly think the aim of my story is to try and help other people in similar situations. Things aren’t perfect and probably never will be, but things are good and I am a good mummy to my little boy and he is happy and healthy, despite all that has happened.’
I would like to thank Grace and her courage to share her story and wish her well on her road to recovery. Recovery is never easy but is possible.
For more information take a look at the websites below
Mind
Rethink
pre and postnatal depression advice and support
Postnatal illness
[i] http://www.nhs.uk/news/2011/10October/Pages/call-for-postnatal-depression-support.aspx
[ii] http://www.nhs.uk/news/2011/10October/Pages/call-for-postnatal-depression-support.aspx
[iii] http://www.nhs.uk/news/2011/10October/Pages/call-for-postnatal-depression-support.aspx
[iv] Give Me Strength: Suffering in silence – A campaign from 4Children to avert family crisis 70,000 reasons why help with postnatal depression has to be better – page 6
[v] Give Me Strength: Suffering in silence – A campaign from 4Children to avert family crisis 70,000 reasons why help with postnatal depression has to be better – page 6
[vi] Give Me Strength: Suffering in silence – A campaign from 4Children to avert family crisis 70,000 reasons why help with postnatal depression has to be better – page 8
[vii] Give Me Strength: Suffering in silence – A campaign from 4Children to avert family crisis 70,000 reasons why help with postnatal depression has to be better – page 8
 In my short life I have fund-raised for many charities. But Beat is a very important charity to me. The parent helpline helped my mum with finding help and support for me. They have also given me advice when I needed it.
In my short life I have fund-raised for many charities. But Beat is a very important charity to me. The parent helpline helped my mum with finding help and support for me. They have also given me advice when I needed it.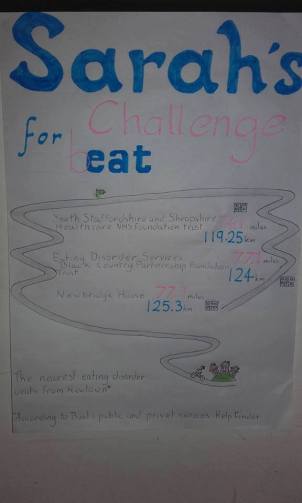 So using Beat’s Help Finder directory of public and private services. Shows that the three closest treatment centres are:
So using Beat’s Help Finder directory of public and private services. Shows that the three closest treatment centres are: On Friday the 26th February there were bucket loads of cake available including healthy and Vegan cakes. I started at 10am and with help from some volunteers in finally made it at 3.20pm I reached the final target of 77.9 miles. To say I was exhausted was an understatement. All the members at Ponthafren counted down with me to each target with a huge round of applause. It was a huge achievement for me and it demonstrates how far someone could possibly have to travel to get specialist help.
On Friday the 26th February there were bucket loads of cake available including healthy and Vegan cakes. I started at 10am and with help from some volunteers in finally made it at 3.20pm I reached the final target of 77.9 miles. To say I was exhausted was an understatement. All the members at Ponthafren counted down with me to each target with a huge round of applause. It was a huge achievement for me and it demonstrates how far someone could possibly have to travel to get specialist help. It’s not the amount of money we raised that counts but the fact we did it! I hope there comes a day when eating disorders are more understood and treatment is easier to access.
It’s not the amount of money we raised that counts but the fact we did it! I hope there comes a day when eating disorders are more understood and treatment is easier to access.





 When people think mental illness, they think Depression, Anxiety, Bipolar, schizophrenia and many more. But people forget that Postnatal Depression (PND) is a mental illness. From speaking to friends who have experienced Postnatal Depression they have been blamed for the illness or have been ignored by family members. Postnatal Depression is not a normal part of child birth. To me this is infuriating, especially as I have seen people go through this. One mother told me that there doctor refused to refer her to local Community Mental Health Team (CMHT) as ‘Postnatal Depression is hormonal and can be treated with medication’. This really doesn’t help with the feeling of they are the one at fault.
When people think mental illness, they think Depression, Anxiety, Bipolar, schizophrenia and many more. But people forget that Postnatal Depression (PND) is a mental illness. From speaking to friends who have experienced Postnatal Depression they have been blamed for the illness or have been ignored by family members. Postnatal Depression is not a normal part of child birth. To me this is infuriating, especially as I have seen people go through this. One mother told me that there doctor refused to refer her to local Community Mental Health Team (CMHT) as ‘Postnatal Depression is hormonal and can be treated with medication’. This really doesn’t help with the feeling of they are the one at fault.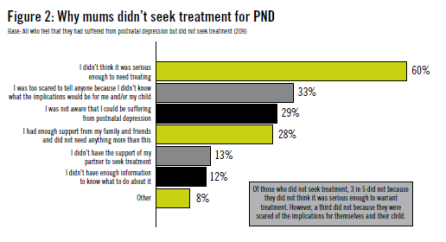 Shockingly 60% percent of those with Postnatal Depression didn’t think it was serious enough to seek treatment. Sadly 33% were too scared to tell anyone because they didn’t know what the implications would be for them and/or their child. 29% didn’t know that they were suffering from postnatal depression.
Shockingly 60% percent of those with Postnatal Depression didn’t think it was serious enough to seek treatment. Sadly 33% were too scared to tell anyone because they didn’t know what the implications would be for them and/or their child. 29% didn’t know that they were suffering from postnatal depression. ‘In the unit, I was given more help and talking therapy. I also to some lovely people some of whom is still keep in touch with. I was discharged after three weeks. When I left the unit, I walked out the door happier and heather with the right medication it also changed my whole perception of mental illness! It really was an eye opener.’
‘In the unit, I was given more help and talking therapy. I also to some lovely people some of whom is still keep in touch with. I was discharged after three weeks. When I left the unit, I walked out the door happier and heather with the right medication it also changed my whole perception of mental illness! It really was an eye opener.’ 










