In the UK it is estimates that 1.2% of the population will have OCD, which equates to 12 out of every 1000 people, based on these statistics, approximately 741,504 people are living with OCD at any one time.[i]
In the UK it is estimates that 1.2% of the population will have OCD, which equates to 12 out of every 1000 people, based on these statistics, approximately 741,504 people are living with OCD at any one time.[i]
50% of all these cases will fall into the severe category, with less than only a quarter being classed as mild cases. Which is why some estimates suggest that maybe 2-3% of all those visiting their GP will be doing so because of OCD.[ii]
It is believed that many people affected by OCD still suffering in silence through embarrassment and fear of being labelled. Others are unaware that their suffering is a recognised medical condition.[iii]
So what is OCD?
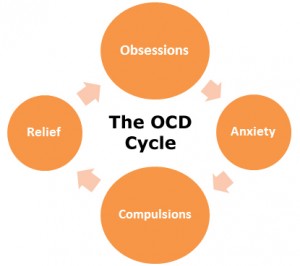
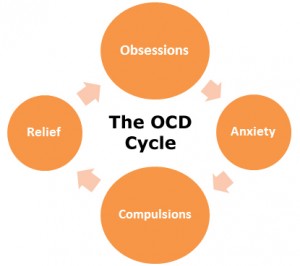 Obsessive-Compulsive Disorder has two main parts. Obsessions and Compulsions. Obsessions are unwelcome thoughts, ideas or urges that repeatedly appear in your mind. Compulsions are repetitive activities that you have to do. The aim of the compulsion is to ‘put right’ the distress caused by the obsessive thoughts and temporarily relive the anxiety you are feeling. It is unlikely that you will feel any pleasure from carrying out the compulsion.[iv]
Obsessive-Compulsive Disorder has two main parts. Obsessions and Compulsions. Obsessions are unwelcome thoughts, ideas or urges that repeatedly appear in your mind. Compulsions are repetitive activities that you have to do. The aim of the compulsion is to ‘put right’ the distress caused by the obsessive thoughts and temporarily relive the anxiety you are feeling. It is unlikely that you will feel any pleasure from carrying out the compulsion.[iv]
Many of us experience minor obsessions or compulsions, approximately four-fifths of us. However, the distinction between this and Obsessive – Compulsive Disorder is its severity. With Obsessive Compulsive Disorder the problems are so sever they interfere with everyday life. It might mean spending eight to ten hours a day washing, with hand red-raw and bleeding. Or it might mean repeatedly dressing and undressing or running up and down stairs.[v]
| Common Obsessions[vi]
|
Common Compulsions[vii]
|
| · Fearing contamination
· Imagining doing harm
· Fearing your aggressive urges
· Intrusive sexual impulses
· Excessive doubts
· ‘forbidden’ thoughts
· Needing things to be perfect
· Needing to confess something
|
· Repeating actions
· Ordering or arranging
· Hoarding or saving
· Washing
· Checking
· Touching
· Counting
· Praying |
Interview this Georgia
I caught up with Georgia who suffers with OCD
“When people think OCD, they think of washing hands, tidying etc. The term OCD is thrown around a lot.”
“OCD feels like a constant state of anxiety, because unless things are organised and they are how your mind wants them to be. Your mind convinces you that anything and everything is going to go wrong.”
“For me my OCD is especially prevalent when things in my life feel out of control, so by organising things and taking control of my physical environment. It makes me feel at least in control of something.”
I asked Georgia about her compulsions and the obsessions behind them and how they affect her.
“One of my regular compulsions is that the sofa has to be in the ‘correct’ position. I can spend up to an hour adjusting and readjusting it until it’s exactly right. If I don’t do it I feel extremely uncomfortable. I won’t be able to settle because everything feels out of balance.”
“My routines are important. An example of his would be every morning I have to as soon as I wake up, I go to the loo, take my medication, then back into bed, then check my tablet and phone, and then I will have a cigarette. If I don’t do it that way the fear is that my whole day will go wrong.”
“My DVD’s are organised in age range (U-18), genre, collections and actors. The fear behind that is if the DVD’S are not in that particular order, the DVD’S wouldn’t work.”
“The intensity of the fear can be as extreme as a panic attack or it can be just feeling unsettled and extremely uncomfortable.”
“As for the urge to carry out the compulsion, it feels like having an itch that you have to scratch.”
“At the time the reason doesn’t occur to me (why I carry out the compulsion) until I really think about it or something interferes with the compulsion. E.g. People moving things in my flat”
I then asked Georgia if she had any tips to cope with the obsessions and compulsions. And here is her advice.
“Being kind to yourself, not having a go at yourself for needing to complete the compulsion.”
“Allocate only a certain amount of time to complete the compulsion so it doesn’t have a huge impact on my day as it could do.”
“Try to rationalise the obsession and look at it realistically ‘is this actually going to ruin my day or upset my friends and family.”
If you think you may have OCD or any other condition. Please see your GP.
[i] http://www.ocduk.org/how-common-ocd 10/08/15
[ii] http://www.ocduk.org/how-common-ocd 10/08/15
[iii] http://www.ocduk.org/how-common-ocd 10/08/15
[iv] mind, understanding Obsessive- Compulsive Disorder leaflet. Page 3
[v] mind, understanding Obsessive- Compulsive Disorder leaflet. Page 4
[vi] mind, understanding Obsessive- Compulsive Disorder leaflet. Page 5
[vii] mind, understanding Obsessive- Compulsive Disorder leaflet. Page 5